
Marc-Olivier GAUCI
Intelligence in Computational and Augmented surgery, Reuse of healthcare data, multiparametric Evaluation (ICARE)
Main interests
- Computation and Augmented Surgery
- Digital model for Surgery application
- Healthcare Data reuse
- Multiparametric Evaluation
Scientific Questions
Digital surgery merges two complementary aspects:
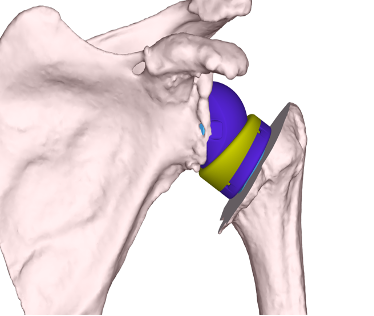
- Computational surgery, which is fed by patient and imaging data, enabling the creation of 3D/4D geometric and biomechanical models to simulate and plan surgery before it is performed.
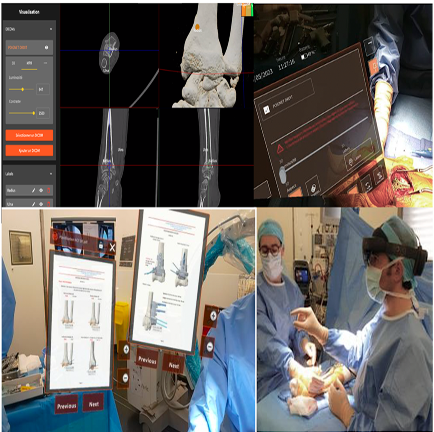
- Augmented surgery, which is based on a more or less complex digital model and enables planning to be applied using intraoperative assistance and guidance tools such as 3D printing (model, instrumentation, implant), navigation, robotics or mixed reality including collaborative cloud platform.
Assessing the clinical relevance of these digital solutions alone is not enough to demonstrate their usability and interest in a complex environment such as the operating room or interventional procedure room. The development of models adapted to surgical needs, and the analysis of multiparametric data derived from the use of these models' application tools, should enable us to optimize the integration of these tools in the operating room and in daily practice.
Our Strategy
The ICARE laboratory's strategy is to create reliable automated numerical models, notably using ML or AI tools, that will be used in the diagnosis, decision making process and surgical procedure. To assess their usability through various application tools, we are carrying out crash tests in real life conditions and developing multi-parametric usability matrices for digital solutions. These results will serve as reliable indicators of a digital tool's ability to integrate into a surgical workflow.
Research Aims
The ICARE laboratory is at the interface between a research and development activity involving researchers and industrial partners, and an application activity carried out by surgeons on test platforms (anatomy laboratory, augmented operating room, simulators) and in operating rooms. The ICARE team is working on 3D model of bone especially shoulder, forearm, distal radius and pelvis in order to provide preoperative reliable and automated model to treat bone fractures. Statistical shape models are also developed to retrieve the premorbid bone and joint and to guide the objective of the surgery.
The ICARE laboratory's activities are part of a 360° assessment of the use of digital tools in the operating room, which is the only way to guarantee their performance. Human factors are considered, whether subjective (mental workload, situational awareness or acceptability) or objective (heart rate, sweating, etc.) during the procedure. We aim to develop indicators to predict the usability of numeric surgical devices.
The use of data generated using digital tools is also at the heart of ICARE's strategy. We are also promoting the industrialization of high-quality data collection to feed our algorithms, in close collaboration with the Côte d'Azur healthcare data warehouse.
Humerus model
Traumatology is a major public health scourge worldwide, and the third leading cause of global morbidity according to the WHO (50% of emergency consultations and 400 000 hospitalizations a year).
Fractures of the proximal humerus are the 3rd most common fracture and therefore represent a major public health issue (loss of independence in the elderly, disability in young, active patients).
We are developing personalized, collaborative preoperative planning for trauma surgery on the proximal humerus to minimize operative complications and recovery time.
This includes:
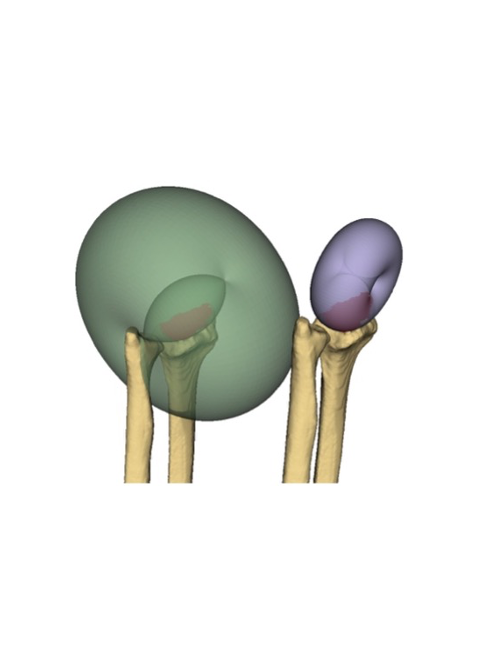
- Creation of a generative model (of the variational auto-encoder or adversarial generative network type) of the proximal humerus fracture, making it possible to generate a representation of a fractured humerus from the representation of an average non-fractured humerus (and vice versa).
- Creation of a generative model (anatomical variability of the humerus)
- Automated segmentation of the fractured head of the humerus from CT images of the shoulder. The difficulty arises from the fragmentation of the humeral head into multiple pieces that vary according to the nature of the fracture.
- Estimating the reduced shape of the proximal humerus
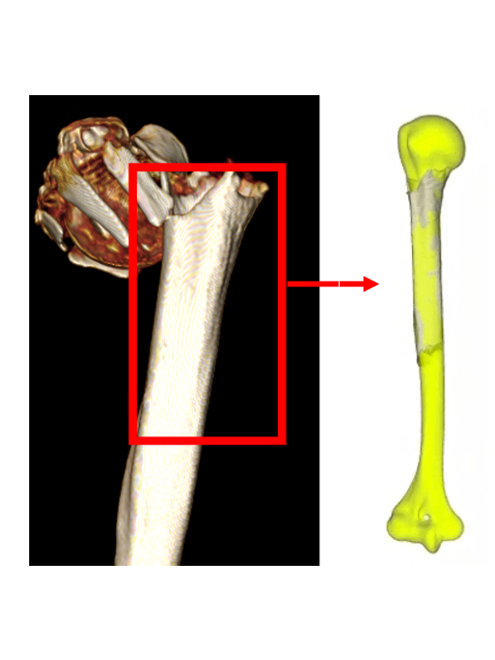
Distal Radius
Fractures of the distal radius account for 20% of all fractures. The diversity of fracture types requires specific management of each patient. We are developing a standard 3D model of the forearm including the distal radius by detecting 3D anatomical reference systems in a reproducible and automatable way to eliminate user dependency on reference system placement and improve joint characterization. There are several applications for the model, such as implementation in software to make a precise diagnosis, guide the therapeutic decision and plan surgery by selecting the most suitable osteosynthesis plates. Intraoperative application is made possible by the generation of 3D-printed patient-specific guides and the use of mixed reality.
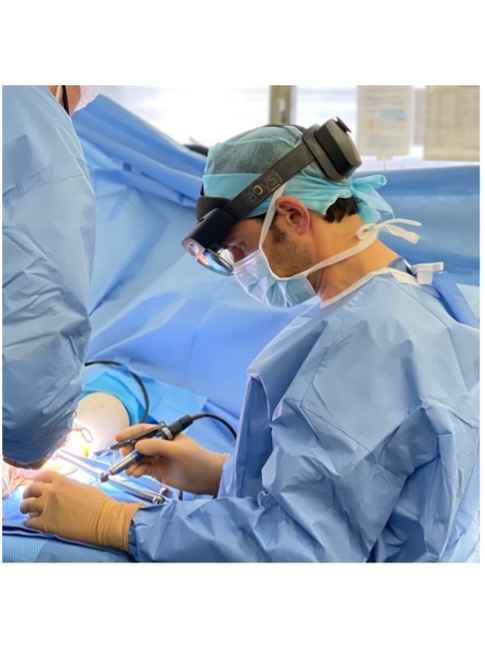
Human factors in the intraoperative use of mixed reality
We aim to investigate the role of physician’s acceptability towards MR and rendering tools and the impact on professionals’ mental workload perception. Indeed, this research investigation will mobilize a conceptual framework grounded on Information System Theory and backed by personal-based characteristics. So, the technological acceptance and individual attitudes (self-efficacy, work relevance, anxiety) are used. Acceptability assessment with adapted scores completes the reflection, reinforcing the understanding of practices and attitudes. Subjective, physiological, and behavioral measures are collected. Structural equation models and generalized additive models are be used to perform associations and causal relationships between variables. This methodological approach is particularly relevant for measuring, estimating, and testing research models and linear and non-linear relations between concepts simultaneously. This methodology is specifically adapted to assess complex models studied in a real-world environment (impacted by causal relationship between variables).

Perioperative (pre-, intra- and post-operative) data collection for translational research: the fraCTure project
Results in orthopedics and trauma surgery is highly related to experience. Orthopedics and Traumatology present specific technological barriers of shortening the time between planning and procedure, reducing sources of errors, internalizing tools and processes of automated planning in the care institutions and of empowering the surgeons.
Through the ongoing Côte d’Azur Health Data Warehouse project, we are building a project to industrialize the collection of data, the data quality enhancement, and the accessibility of the data to make clinical, imaging, and intraoperative necessary data available for 3D models generation for intraoperative evaluation and to associate a longitudinal follow-up of cohorts for clinical validation. For this purpose, we have established a collaboration with the HUGO health data warehouse to continuously collect the data necessary for our research and development. The same solution is used by the Côte d’Azur and the HUGO Health data Warehouse, to facilitate interactions. The final goal is to associate multiple EDS in trauma centers and well-recognized and high-volume orthopedics facilities to build an efficient network to collect data around surgery. Multiple innovative approaches such as federated learning are relevant and has been already applied in other fields (cancerology).
A specific focus is done for intraoperative data collected through mixed reality use.
Clinical Researchers
 AMORETTI Nicolas - +33 493377798
AMORETTI Nicolas - +33 493377798 GONZALEZ Jean-François - +33 A
GONZALEZ Jean-François - +33 A MICICOI Grégoire - +33 A
MICICOI Grégoire - +33 A BERNARD DE DOMPSURE Régis - +33 A
BERNARD DE DOMPSURE Régis - +33 A D'ASCOLI Alessander - +33 A
D'ASCOLI Alessander - +33 A MASSALOU Damien - +33 A
MASSALOU Damien - +33 A RANC Pierre-Alexis - +33 A
RANC Pierre-Alexis - +33 A BRONSARD Nicolas - +33 A
BRONSARD Nicolas - +33 A DOUIRI Adil - +33 A
DOUIRI Adil - +33 A ALLIA Jeremy - +33 A
ALLIA Jeremy - +33 A SOLLA Frederico - +33 R
SOLLA Frederico - +33 R CHOPLIN Arnaud - +33 489153891
CHOPLIN Arnaud - +33 489153891 FORESTIER Emilie - +33 R
FORESTIER Emilie - +33 R AMORETTI Nicolas - +33 R
AMORETTI Nicolas - +33 R DE DOMPSURE Régis - +33 R
DE DOMPSURE Régis - +33 R FAUCHILLE Tristan - +33 R
FAUCHILLE Tristan - +33 R
PreDocs
 LOPEZ NORENA Vanessa - +33 R
LOPEZ NORENA Vanessa - +33 R LOPEZ NORENA Vanessa - +33 R
LOPEZ NORENA Vanessa - +33 R BADINA Alina - +33
BADINA Alina - +33  CAUBERE Alexandre - +33 483162453
CAUBERE Alexandre - +33 483162453 ARMINIO Marie - +33 R
ARMINIO Marie - +33 R DE LANGLAIS Alix - +33 R
DE LANGLAIS Alix - +33 R
Engineers & Technicians
 AGUILAR VIDAL Théo - +33 R
AGUILAR VIDAL Théo - +33 R COSTANTINI Isa - +33 4 92 03 70 27
COSTANTINI Isa - +33 4 92 03 70 27 SREEDHAR Hari - +33 R
SREEDHAR Hari - +33 R BRAHIM Abdelbasset - +33 R
BRAHIM Abdelbasset - +33 R LOPEZ Stéphanie - +33 R
LOPEZ Stéphanie - +33 R WANG Zhe - +33 R
WANG Zhe - +33 R
Students
 BOULY Noé - +33 R
BOULY Noé - +33 R
Recent publications
- Caubère, A, Vervaecke, AJ, Jung, A, Werthel, JD, Gauci, MO, Boux de Casson, F et al.. Total shoulder arthroplasty preoperative planning: Does the patient's arm position in the CT-scan affect posterior humeral head subluxation?. Orthop Traumatol Surg Res. 2026; :104635. doi: 10.1016/j.otsr.2026.104635. PubMed PMID:41651063 .
- Joshi, S, Njessi, P, Camuzard, O, Gauci, MO, Bonvalot, S, Lupon, E et al.. The emerging role of mixed reality and artificial intelligence in sarcoma care: A systematic review. Eur J Surg Oncol. 2026;52 (3):111447. doi: 10.1016/j.ejso.2026.111447. PubMed PMID:41643627 .
- Rios, O, Gauci, MO, Debortoli, C, Alunni, V, Savoldelli, C. A 3D-printed craniofacial fracture library with QR-integrated pedagogical content: a technical note for maxillofacial trauma teaching. J Stomatol Oral Maxillofac Surg. 2026;127 (4):102736. doi: 10.1016/j.jormas.2026.102736. PubMed PMID:41619937 .
- Vervaecke, AJ, Gauci, MO, Le Brigand, J, Verborgt, O, Werthel, JD, Caubère, A et al.. SECEC Grammont Award 2025: The resting arm position influences impingement-free range of motion and the distalization and lateralization shoulder angle in reverse shoulder arthroplasty preoperative planning. J Shoulder Elbow Surg. 2026; :. doi: 10.1016/j.jse.2025.12.014. PubMed PMID:41577229 .
- Giovannetti de Sanctis, E, Monin, B, Bronsard, N, Gonzalez, JF, Gauci, MO. The Neviaser approach for proximal humerus fractures third-generation intramedullary nailing: A cadaver study. Orthop Traumatol Surg Res. 2025; :104577. doi: 10.1016/j.otsr.2025.104577. PubMed PMID:41429269 .
- Giovannetti de Sanctis, E, Gauci, MO. Response to correspondence: Commentary on Muscle-Sparing approaches in reverse shoulder arthroplasty. Int Orthop. 2026;50 (1):347-349. doi: 10.1007/s00264-025-06725-8. PubMed PMID:41369903 .
- Giovannetti de Sanctis, E, Bige, B, Cornacchini, J, Bronsard, N, Gonzalez, JF, Gauci, MO et al.. Three-part proximal humerus fracture: a full-percutaneous severely displaced greater tuberosity reduction and intramedullary nailing technique. JSES Rev Rep Tech. 2025;5 (4):1129-1137. doi: 10.1016/j.xrrt.2025.05.016. PubMed PMID:41179400 PubMed Central PMC12573496.
- Giovannetti de Sanctis, E, Jacquot, A, Bronsard, N, Gonzalez, JF, Gauci, MO. Comparison of Anterior Muscle Sparing (AMS) approach and conventional subscapularis tenotomy - repair for deltopectoral approach in reverse shoulder arthroplasty: is there more complications and implant malposition?. Int Orthop. 2025;49 (11):2685-2695. doi: 10.1007/s00264-025-06665-3. PubMed PMID:41065821 .
- Roy, C, Berhouet, J, Jacquot, A, Werthel, JD, Gauci, MO. Interobserver concordance analysis for the evaluation of internal rotation with elbow at the side during shoulder clinical examination. Orthop Traumatol Surg Res. 2025; :104427. doi: 10.1016/j.otsr.2025.104427. PubMed PMID:40953698 .
- Vervaecke, AJ, Ricciardi, B, Boux de Casson, F, Blancheton, A, Housset, V, Caubère, A et al.. The influence of humeral implant alignment on the arm position in the coronal plane after reverse total shoulder arthroplasty. Int Orthop. 2025;49 (11):2697-2705. doi: 10.1007/s00264-025-06650-w. PubMed PMID:40938414 .
- Caubère, A, Rutigliano, S, Bourdon, S, Erickson, J, Morelli, M, Parsons, M et al.. How does subscapularis repair affect joint loads? Effect of humeral tray thickness in Reverse Total Shoulder Arthroplasty (rTSA). Orthop Traumatol Surg Res. 2025; :104413. doi: 10.1016/j.otsr.2025.104413. PubMed PMID:40921265 .
- Bige, B, Recanatesi, N, Gonzalez, JF, Gauci, MO. Combined Hill-Sachs remplissage and Latarjet procedure: does glenoid track help decision making?. JSES Int. 2025;9 (4):1048-1054. doi: 10.1016/j.jseint.2025.03.014. PubMed PMID:40703418 PubMed Central PMC12281291.
- Caubère, A, Boux de Casson, F, Jung, A, Werthel, JD, Vervaecke, AJ, Gauci, MO et al.. Total shoulder arthroplasty preoperative planning: the effect of patient's humeral position on the lateralization and distalization measurements. Int Orthop. 2025;49 (9):2111-2122. doi: 10.1007/s00264-025-06619-9. PubMed PMID:40690017 .
- Gauci, MO, De Geofroy, B, Chamoux, J, Bige, B. Erratum to 'Posterior Unstable And Painful Shoulders (P-UPS) Are Associated With Low Posterior Acromial Coverage And Increased Posterior Humeral Subluxation.' [JSES International Volume 6 Issue (2024) Page 1368]. JSES Int. 2025;9 (3):999. doi: 10.1016/j.jseint.2024.11.013. PubMed PMID:40486773 PubMed Central PMC12144975.
- Winter, R, Poujade, T, Monin, B, Viricel, C, Bronsard, N, Chabrand, P et al.. Validation of an automatic three-dimensional method for distal radius measurements and malunion quantification. J Hand Surg Eur Vol. 2025;50 (10):1371-1378. doi: 10.1177/17531934251340240. PubMed PMID:40376982 .
- Collotte, P, Gauci, MO, Vieira, TD, Walch, G. Corrigendum to 'Bony increased-offset reverse total shoulder arthroplasty (BIO-RSA) associated with an eccentric glenosphere and an onlay 135° humeral component: clinical and radiological outcomes at a minimum 2-year follow-up' [JSES International Volume 6, Issue 3 (2022) 434-441]. JSES Int. 2025;9 (2):601. doi: 10.1016/j.jseint.2024.10.001. PubMed PMID:40182278 PubMed Central PMC11962535.
- D'Ascoli, A, Giovannetti de Sanctis, E, Bronsard, N, Gauci, MO, Gonzalez, JF. Both Isolated Long Head of the Biceps Tenotomy and Tenodesis Are Effective for Symptomatic Rotator Cuff Repair Revision. J Clin Med. 2025;14 (3):. doi: 10.3390/jcm14030852. PubMed PMID:39941523 PubMed Central PMC11818303.
- Jacquot, A, Cuinet, T, Peduzzi, L, Wong, P, Gauci, MO, Uhring, J et al.. Deltopectoral approach without subscapularis detachment for reverse shoulder arthroplasty. Technique and results of a safe and reproducible subscapularis-sparing approach. JSES Rev Rep Tech. 2025;5 (1):14-21. doi: 10.1016/j.xrrt.2024.09.006. PubMed PMID:39872348 PubMed Central PMC11764111.
- de Geofroy, B, Fauchille, T, Djian, M, Gauci, MO, Bohic, JY, Pocquet, X et al.. Individualized total knee arthroplasty achieves better functional results than off-the-shelf implants in patients undergoing personalized coronal alignment. Knee. 2025;53 :228-235. doi: 10.1016/j.knee.2024.12.009. PubMed PMID:39864114 .
- Gauci, MO, Caubere, A, Bronsard, N, Jacquot, A, Berhouet, J, Gonzalez, JF et al.. Anatomic total shoulder arthroplasty with keeled glenoids in patients younger than 60 years at 10 years minimum: which risk factors of failure are still valid at long-term follow-up?. J Shoulder Elbow Surg. 2025;34 (8):e611-e620. doi: 10.1016/j.jse.2024.11.039. PubMed PMID:39855334 .
2022 - CAOS International Best Communication
2020 - Award Innovation days EIT Health, Institut 3IA, (artificial intelligence)
2018 - French Orthopaedic and Traumatology Surgery College Medal
2017 - Price of the Université Côte d’Azur
2016 - Price of the French Academy of Surgery (Labex Cami), Computer Assisted Surgery
2015 - Gold Medal of University Hospital Center of Nice, Surgeon field
2014 - Best Communication Prize, SOFCOT
iBV - Institut de Biologie Valrose
"Tour Pasteur"
Université Nice Sophia Antipolis
Faculté de médecine
28 Avenue de Valombrose
06189 Nice cedex 2
